文章信息
- 庞海清, 潘莉, 宋红梅
- PANG Haiqing, PAN Li, SONG Hongmei
- 艾盐包热熨膻中穴治疗产后郁滞期乳痈患者的效果观察
- Effect observation of moxa-salt ironing at Danzhong(CV17) point treat with post-partum acute mastitis in stagnation period
- 天津中医药, 2021, 38(10): 1312-1315
- Tianjin Journal of Traditional Chinese Medicine, 2021, 38(10): 1312-1315
- http://dx.doi.org/10.11656/j.issn.1672-1519.2021.10.18
-
文章历史
- 收稿日期: 2021-03-25
乳痈是产后常见疾病,相当于西医中的急性乳腺炎[1]。郁滞期乳痈是乳痈的发生早期,以乳房胀痛、乳房肿块、乳汁分泌不畅或伴恶寒发热为主要临床表现[2]。此时,乳房局部尚未形成脓肿,若失于调治或治法不当,极易腐化酿脓,导致哺乳期妇女过早回乳,直接影响母乳喂养[3]。中医认为,及早疏通乳络、排除宿乳是产后郁滞期乳痈治疗的关键[4]。艾盐包热熨穴位是一种全新的灸疗方式,可利用温热效力将艾草药性透过体表毛窍达到血脉、经络,进而发挥温中驱寒、活血化瘀、通经活络之功效[5]。本研究采用艾盐包热熨膻中穴治疗产后郁滞期乳痈,取得满意效果,现报道如下。
1 资料与方法 1.1 一般资料选取2016年7月—2018年12月海南省中医院妇产科收治的148例产后郁滞期乳痈患者为研究对象。纳入标准:1)符合《中医外科学》[6]制定的郁滞期乳痈诊断标准。2)年龄18~40岁。3)哺乳期妇女。4)知情同意并签署知情同意书。排除标准:1)体温>38.5 ℃。2)乳房局部皮肤出现湿疹、破溃、糜烂,B超示局部脓肿。3)合并糖尿病、心脑血管疾病、肝肾疾病、血液系统疾病等严重性疾病者。4)对受试药物无法耐受者。5)乳房假体植入者。按随机数字表法将148例患者分为对照组和观察组,每组74例。对照组年龄20~40岁,平均年龄(28.2±5.6)岁;初产妇51例,经产妇23例;顺产40例,剖宫产34例;单侧乳痈55例,双侧19例;观察组年龄19~40岁,平均年龄(27.9±5.0)岁;初产妇48例,经产妇26例;顺产43例,剖宫产31例;单侧乳痈54例,双侧20例。两组患者一般资料比较无统计学差异(P>0.05),具有可比性。
1.2 方法 1.2.1 对照组给予常规护理,包括抗炎治疗、手法按摩、局部热敷等。
1.2.2 观察组在对照组基础上给予艾盐包热熨膻中穴,具体操作如下:取粗盐300 g与艾绒100 g搅拌混匀,装于厚棉布袋中并包扎成直径约10 cm、高约5 cm的圆盘状艾盐包备用;取艾盐包,在其表面喷少量水至棉布微潮,置于微波炉内,调至中火加热3 min取出,艾盐包温度约45~50 ℃;嘱患者取仰卧位,将加热后的艾盐包敷于膻中穴,温度以患者感觉不烫伤皮肤为宜,热熨30 min左右。10 d为1个疗程。
1.3 评价指标 1.3.1 症状积分分别于治疗前后,参照《中药新药临床研究指导原则》评价患者临床症状体征[7]。乳房肿块:无肿块计0分,肿块长径≤2 cm计1分,2 cm<肿块长径≤4 cm计2分,肿块长径>4 cm计3分;乳房胀痛:无胀痛计0分,轻微胀痛计1分,胀痛明显但尚可忍受计2分,胀痛强烈、无法忍受计3分;乳汁分泌不畅:乳汁分泌正常计0分,乳汁分泌欠通畅计1分,乳汁分泌不通畅计2分,乳汁点滴而下或完全无法排出或淤积结块计3分。
1.3.2 临床疗效于治疗结束后参考文献[8]评价治疗效果。痊愈:临床症状、体征完全消失,乳汁分泌正常;显效:临床症状、体征明显好转,肿块减少>60%;有效:临床症状、体征好转,肿块减少>30%;无效:临床症状、体征无改善,甚至恶化。
1.3.3 血清学指标分别于治疗前后,采集患者清晨空腹肘静脉血,常规分离血清,采用酶联免疫吸附(ELISA)法检测血清中肿瘤坏死因子-α(TNF-α)、C反应蛋白(CRP)水平变化。
1.4 统计学分析使用SPSS 23.0分析数据,计量资料用均数±标准差(x±s)表示,组内前后比较采用配对t检验,组间比较采用两独立样本t检验;计数资料用构成比或率表示,组间比较采用χ2检验,P<0.05表示具有统计学差异。
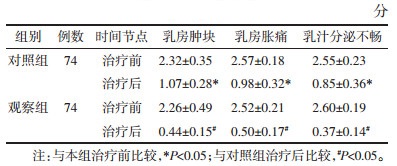
2 结果 2.1 症状积分治疗前,两组各项症状积分比较无统计学差异(P>0.05)。治疗后,两组各项症状积分均较治疗前降低,且观察组低于对照组,差异有统计学意义(P<0.05)。见表 1。
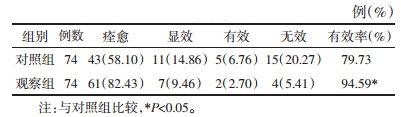
观察组治疗有效率为94.59%,显著高于对照组的79.73%,差异有统计学意义(P<0.05)。见表 2。
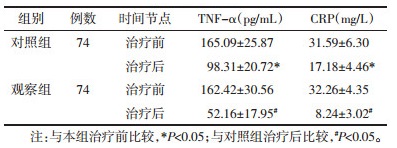
治疗前,两组血清TNF-α、CRP水平比较无统计学差异(P>0.05)。治疗后,两组血清TNF-α、CRP水平均较治疗前显著降低,且观察组低于对照组,差异有统计学意义(P<0.05)。见表 3。
中医认为,乳汁郁积、乳络不通是产后乳痈的主要病机。产后饮食不节、外邪入侵、胃热壅滞、肝气郁结,可致乳汁蓄积,宿乳使乳络失宣,乳汁郁久化热酿毒,毒盛内腐而成脓[9]。产后乳痈分为郁滞期、化脓期、溃后期3期,具有发病急、进展快、易成脓破溃等。因此,产后郁滞期乳痈的治疗原则应以“温通”为用,尤贵于早[10]。
3.2 艾盐包热熨膻中穴治疗产后郁滞期乳痈的效果本研究结果显示,相较于对照组,观察组治疗后乳房肿块、乳房胀痛、乳汁分泌不畅积分明显降低(P<0.05);且观察组治疗有效率较对照组显著提高(P<0.05),提示艾盐包热熨膻中穴治疗产后郁滞期乳痈效果显著。
艾盐包以艾叶和粗盐为主要成分。艾叶性温,味苦、辛,入肝、肾、脾3经,具有通经活络、温中理气、行气活血、祛寒止痛之功效。粗盐性寒,味咸,可清热解毒、活血化瘀,且兼具保温性能,可增强药物疗效。艾盐包热熨疗法是借助艾盐加热后的温热之力,使药效能透过皮肤毛孔透皮吸收,由表及里,直达经络、血脉[11]。周静等[12]研究发现,艾盐包热熨能有效减轻甘露醇注射时的疼痛,降低甘露醇致静脉炎的发生率,其效果优于温毛巾热敷。膻中穴归属任脉,是中医治疗乳腺疾病的重要穴位之一,刺激该穴可调理全身气机,使气血调和、经络通利。艾盐包热熨膻中穴可起到温通经络、消炎止痛、活血化瘀,与产后郁滞期乳痈的治疗原则不谋而合,从而达到减轻产后郁滞期乳痈临床症状,提高临床疗效的效果。
3.3 艾盐包热熨膻中穴治疗产后郁滞期乳痈的机制本研究结果显示,相较于对照组,观察组治疗后血清TNF-α、CRP水平明显降低(P<0.05)。TNF-α是公认的促炎因子,可诱导多种炎症介质合成与分泌,进而介导炎症级联反应[13]。血清CRP水平可直接反映机体炎症反应程度[14]。研究指出,产后郁滞期乳痈患者血清TNF-α、CRP水平出现明显的上调[15]。穴位疗法的抗炎作用以得到普遍公认。李斌等[16]研究显示,刺激穴位通过调节白细胞介素(IL)-5、IL-10等炎症因子水平,支气管哮喘患者降低气道炎症,改善临床症状。本研究结果表明,艾盐包热熨膻中穴可降低产后郁滞期乳痈患者血清TNF-α、CRP水平,发挥显著的抗炎作用。究其原因,可能与艾盐包热熨膻中穴可温通经络,改善乳房胀痛,促进乳汁分泌,清除患处乳汁瘀滞有关,从而减轻了局部炎症反应,这可能也是其治疗产后郁滞期乳痈的主要机制。
综上所述,艾盐包热熨膻中穴治疗产后郁滞期乳痈,可显著改善临床症状,提高临床疗效,其主要机制可能与抑制血清炎症因子水平有关。
| [1] |
张董晓, 赵文洁, 付娜, 等. 中医古籍"乳痈"证治探析[J]. 长春中医药大学学报, 2017, 33(1): 151-153. ZHANG D X, ZHAO W J, FU N, et al. Analysis of the syndrome and treatment of "acute mastitis" in traditional Chinese medicine ancient books[J]. Journal of Changchun University of Chinese Medicine, 2017, 33(1): 151-153. |
| [2] |
李荣娟, 葛建立, 张欣, 等. 耳穴压豆配合拔罐治疗早期乳痈临床观察[J]. 四川中医, 2015, 4(10): 164-165. LI R J, GE J L, ZHANG X, et al. Clinical observation on the treatment of early breast carbuncle by auricular pressure and cupping[J]. Journal of Sichuan Traditional Chinese Medicine, 2015, 4(10): 164-165. |
| [3] |
刘兴静, 周敏, 徐浩娟. 通乳方与瓜蒌牛蒡汤治疗乳痈初期疗效比较[J]. 长春中医药大学学报, 2016, 32(5): 1005-1007. LIU X J, ZHOU M, XU H J. Tongru Decoction and Gualou Niubang Decoction in treatment of early acute mastitis[J]. Journal of Changchun University of Chinese Medicine, 2016, 32(5): 1005-1007. |
| [4] |
毕广东. 近十年国内对中医药治疗哺乳期乳腺炎研究概况[J]. 四川中医, 2016, 3(2): 219-221. BI G D. Research survey of traditional Chinese medicine has treated lactational mastitis in recent ten years[J]. Journal of Sichuan Traditional Chinese Medicine, 2016, 3(2): 219-221. |
| [5] |
潘晓晓. 艾盐包热熨治疗索拉非尼片相关腹泻的疗效观察[J]. 上海针灸杂志, 2018, 37(9): 1011-1012. PAN X X. Therapeutic observation of moxa-salt hot compress for sorafenib-induced diarrhea[J]. Shanghai Journal of Acupuncture and Moxibustion, 2018, 37(9): 1011-1012. |
| [6] |
陆德铭. 中医外科学[M]. 上海: 上海科学技术出版社, 1997: 85-86. LU D M. Traditional Chinese medicine surgery[M]. Shanghai: Shanghai Science and Technology Press, 1997: 85-86. |
| [7] |
陶颖娜, 万华, 仲姗姗, 等. 乳痈方调节乳腺菌群治疗哺乳期乳腺炎的临床研究[J]. 上海中医药杂志, 2018, 52(5): 46-47. TAO Y N, WAN H, ZHONG S S, et al. Clinical study on Ruyong Formula in treating lactational mastitis by regulating mammary gland flora[J]. Shanghai Journal of Traditional Chinese Medicine, 2018, 52(5): 46-47. |
| [8] |
杨香华, 朱仡, 朱炜. 火龙灸联合穴位贴敷治疗产后郁滞期乳痈患者的效果观察[J]. 护理学报, 2016, 23(9): 65-66. YANG X H, ZHU Y, ZHU W. Observation on the effect of fire-dragon moxibustion combined with acupoint application in the treatment of postpartum breast carbuncle[J]. Journal of Nursing, 2016, 23(9): 65-66. |
| [9] |
付晓敏. 针刺、推拿联合中药治疗产后早期乳痈的疗效[J]. 光明中医, 2016, 31(9): 1287-1288. FU X M. Acupuncture and massage combined with traditional Chinese medicine in the treatment of early postpartum mammary carbuncle[J]. Guangming Journal of Chinese Medicine, 2016, 31(9): 1287-1288. DOI:10.3969/j.issn.1003-8914.2016.09.040 |
| [10] |
汪永坚, 王舒洁, 陈晓洁. 扶阳罐循经温刮干预郁滞期乳痈疗效观察[J]. 上海针灸杂志, 2018, 37(10): 1165-1166. WANG Y J, WANG S J, CHEN X J. Therapeutic observation of warm scraping along meridian with yang supporting cup for acute mastitis in stagnation period[J]. Shanghai Journal of Acupuncture and Moxibustion, 2018, 37(10): 1165-1166. |
| [11] |
蔡亚红, 吴育红, 叶富英. 艾盐包热熨中脘穴防治顺铂化疗所致消化道反应的临床研究[J]. 中国针灸, 2016, 36(4): 405-408. CAI Y H, WU Y H, YE F Y. Moxa salt packets at zhongwan (CV12) for cisplatin chemotherapy-induced gastrointestinal reactions: a clinical study[J]. Chinese Acupuncture & Moxibustion, 2016, 36(4): 405-408. |
| [12] |
周静, 孟登科. 艾盐热敷联合推熨预防甘露醇致静脉炎效果观察[J]. 护理学杂志, 2018, 33(13): 33-34. ZHOU J, MENG D K. Prevention of mannitol-induced phlebitis through moxa-salt hot compression combining massage[J]. Journal of Nursing Science, 2018, 33(13): 33-34. DOI:10.3870/j.issn.1001-4152.2018.13.033 |
| [13] |
林小颜, 罗建国, 胡珊, 等. 加味阳和汤联合三苯氧胺对浆细胞性乳腺炎患者炎性因子及免疫功能的影响[J]. 现代中西医结合杂志, 2018, 27(17): 24-26. LIN X Y, LUO J G, HU S, et al. Effect of Jiawei Yanghe Decoction combined with tamoxifen on the immune function and inflammatory factors in patients with plasma cell mastitis[J]. Modern Journal of Integrated Traditional Chinese and Western Medicine, 2018, 27(17): 24-26. |
| [14] |
沈胡刚, 彭志坚, 朱怡平, 等. 散清消通法对早期哺乳期急性乳腺炎患者血WBC、CRP、PCT的影响[J]. 中国中医急症, 2017, 26(9): 1671-1673. SHEN H G, PENG Z J, ZHU Y P, et al. Effect of the treatment-removing stasis, clearing away heat, detumescence and lactogenesis on WBC, CRP and PCT of the blood in patients with acute mastitis at early lactation stage[J]. Journal of Emergency in Traditional Chinese Medicine, 2017, 26(9): 1671-1673. DOI:10.3969/j.issn.1004-745X.2017.09.054 |
| [15] |
朱雪琼, 米海霞, 林祥, 等. 瓜蒌牛蒡汤合阳和汤联合中药外敷对哺乳期急性乳腺炎早期患者IL-6、CRP水平的影响研究[J]. 中华中医药学刊, 2017, 35(4): 819-821. ZHU X Q, MI H X, LIN X, et al. Effects of Gualou Niubang Decoction and Yanghe Decoction combined with external application of Chinese medicine on IL-6 and CRP of patients with acute lactational mastitis in early stage[J]. Chinese Archives of Traditional Chinese Medicine, 2017, 35(4): 819-821. |
| [16] |
李斌, 谢俊刚, 陈奇志, 等. 穴位疗法对支气管哮喘缓解期患者炎症因子及临床疗效的影响[J]. 中华物理医学与康复杂志, 2016, 38(12): 920-923. LI B, XIE J G, CHEN Q Z, et al. Acupoint therapy can reduce airway inflammation and control asthma symptoms[J]. Chinese Journal of Physical Medicine and Rehabilitation, 2016, 38(12): 920-923. DOI:10.3760/cma.j.issn.0254-1424.2016.12.011 |
 2021, Vol. 38
2021, Vol. 38