文章信息
- 姜晨, 宋玉, 吕阳, 杨洪涛
- JIANG Chen, SONG Yu, LYU Yang, YANG Hongtao
- 尿毒症腹膜透析伴血管钙化患者中医证候特征研究
- Study on characteristics of TCM syndrome in uremia patients with peritoneal dialysis complicated with vascular calcification
- 天津中医药, 2021, 38(9): 1144-1148
- Tianjin Journal of Traditional Chinese Medicine, 2021, 38(9): 1144-1148
- http://dx.doi.org/10.11656/j.issn.1672-1519.2021.09.12
-
文章历史
- 收稿日期: 2021-03-30
2. 菏泽市中医医院肾病科, 荷泽 274000;
3. 天津中医药大学第二附属医院急诊科, 天津 300250
血管钙化是慢性肾功能衰竭尿毒症期患者常见和难治的并发症,是导致尿毒症患者心血管疾病的重要诱因[1],也是透析患者全因死亡及心血管事件死亡的独立预测因子[2]。腹膜透析(PD)是尿毒症患者肾脏替代治疗方法之一,目前越来越多终末期肾脏病患者选择PD治疗。而在腹膜透析患者中血管钙化发病率高达65.1%[3],严重危害透析患者生命安全。有效防治血管钙化是提高PD患者生存率的重要途径,然而目前临床尚无有效药物干预和治疗血管钙化。近年来中医药治疗血管钙化逐渐成为研究热点,而中医药治疗该病的临床依据较少,辨证论治缺乏证据支持。本研究探讨尿毒症腹膜透析合并血管钙化患者的中医证候特征及规律,为中医药防治血管钙化提供新的证据与思路。
1 资料与方法 1.1 一般资料筛选2016年1月1日—2018年12月31日在天津中医药大学第一附属医院肾病科规律腹膜透析的尿毒症患者421例,共纳入合并血管钙化合格病例125例,年龄在40~80岁,所有患者均自愿参加本研究,签署知情同意书。
1.2 血管钙化的诊断标准根据2017年改善全球肾脏病预后(KDIGO)组织的慢性肾脏病矿物质和骨异常(CKD-MBD)指南[4]建议,采用腹部侧位平片评价腹主动脉钙化,超声心动图评估心脏瓣膜钙化。其中腹主动脉钙化的评估采用24分半定量方法[5],即根据腹主动脉前壁、后壁钙化的范围分别给予0~3分,≥1分即可认为存在腹主动脉钙化。心脏瓣膜钙化的评估采用超声心动图,即在1个或多个心脏瓣膜上发现>1mm的强回声,即可诊断为瓣膜钙化。
1.3 纳入标准1)尿毒症维持性腹膜透析患者。2)透析龄≥3个月。3)符合K/DIGO的CKD-MBD指南血管钙化诊断标准。4)年龄18~80岁。5)自愿参加本研究,签署知情同意书。
1.4 排除标准1)既往或目前长期接受血液透析治疗的患者。2)合并有原发性甲旁亢、营养不良等其他引起钙磷代谢紊乱的相关疾病者。3)合并有难以纠正或危及生命的心力衰竭、肝功能衰竭、感染、恶性肿瘤等并发症者。4)妊娠或哺乳期妇女。5)有精神行为异常,且不能配合完成证候采集和量表者。
1.5 观察项目收集尿毒症腹膜透析合并血管钙化患者的性别、年龄、透析龄、血肌酐、尿素、电解质、血红蛋白、血浆白蛋白等基本临床要素、钙化情况及中医证候信息,中医证候评价标准参照《中药新药临床研究指导原则》[6]进行辨证分型,总结分析其证候规律,并进一步探讨临床要素与证候分布规律的相关性。
1.6 统计学方法采用SPSS24.0软件进行统计学分析。计量资料采用均值±标准差(x±s)表示;计数资料采用构成比或率表示,组间构成比或率的比较采用卡方检验或Fisher精确概率检验。P<0.05为差异有统计学意义。
2 结果 2.1 一般资料根据纳入及排除标准,本研究共纳入维持性腹膜透析合并血管钙化患者125例,占该时间段内本中心全体维持性腹膜透析患者总数的29.70%。其中男76例(60.80%),女49例(39.20%);平均年龄(68.02±9.06)岁,平均透析龄(30.71±15.46)个月;原发病为主要为肾小球肾炎62例(49.60%),其次糖尿病46例(39.80%),高血压病15例(12.00%),其他2例(1.60%)。125例PD患者中单纯心脏瓣膜钙化者100例(80.00%),单纯腹主动脉钙化8例(6.40%),合并心脏瓣膜和腹主动脉钙化者17例(13.60%);在心脏瓣膜钙化患者中,单纯主动脉瓣钙化90例(76.90%),二尖瓣钙化7例(6.00%),合并主动脉瓣和二尖瓣钙化共20例(17.10%)。
2.2 中医辨证分型情况125例患者均可辨为本虚证,其中109例患者可辨为本虚证合并标实证。本虚证以脾肾阳虚证为主,共66例(48.00%),其次为气阴两虚证25例(20.00%)、脾肾气虚证22例(17.60%)、肝肾阴虚证10例(8.0%)和阴阳两虚证8例(6.40%);标实证以湿热证为主,共54例(49.54%),其次为湿浊证29例(26.61%)、血瘀证17例(15.60%)、水气证8例(7.34%)。
2.3 不同年龄、性别及透析龄的中医证型分布差异情况125例患者的中位年龄为66岁,据此分为两组,分析不同年龄患者的中医证型分布差异情况。结果显示两组患者本虚证分布差异有统计学意义(P < 0.05),标实证分布差异有统计学意义(P < 0.05)。不同性别患者本虚证和标实证分布均差异无统计学意义(P > 0.05)。按照中位透析龄26个月分为两组,结果显示两组患者本虚证分布差异有统计学意义(P < 0.05),两组患者标实证分布差异有统计学意义(P < 0.05)。提示患者年龄、透析龄对中医证候辨别有影响,辨证论治时应考虑患者年龄和透析龄的特点。见表 1。
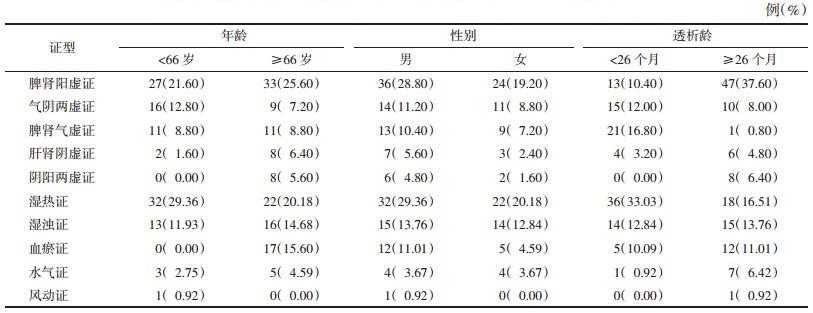
|
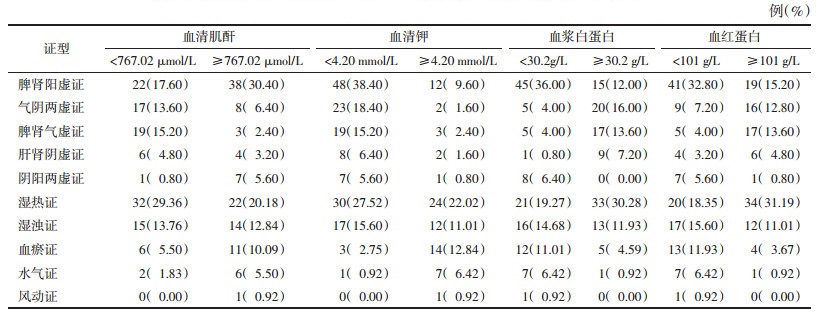
按照中位血清肌酐767.02 μmol/L分为两组,两组患者本虚证分布差异有统计学意义(P < 0.05),标实证分布差异无统计学意义(P > 0.05)。提示本虚证各证型的分布在血肌酐水平上差异有统计学意义(P < 0.05),肌酐偏低时本虚证各种证型分布较平均;而肌酐水平越高,以脾肾阳虚为主的本虚证愈突出;按中位血清钾为4.20 mmol/L分为两组,两组患者本虚证分布差异无统计学意义(P > 0.05),标实证分布差异有统计学意义(P < 0.05)。提示血钾水平影响标实证的辨证分组;按中位血浆白蛋白30.2 g/L分为两组,两组患者本虚证分布差异有统计学意义(P < 0.05),标实证分布差异有统计学意义(P < 0.05)。按照中位血红蛋白101 g/L分为两组,两组患者本虚证分布差异有统计学意义(P < 0.05),标实证分布差异有统计学意义(P < 0.05)。由此说明白蛋白、血红蛋白水平是影响辨证分型的重要因素,提示患者营养状况对临床辨证有重要参考意义。见表 2。
|
研究显示本中心尿毒症PD患者血管钙化的发生率较高(29.7%)。其中单纯心脏瓣膜钙化患者居多(80.0%),同时存在心脏瓣膜及腹主动脉钙化患者次之(13.6%),单纯腹主动脉钙化者较少(6.4%);心脏瓣膜钙化者中单纯主动脉瓣钙化最多(76.9%),同时存在主动脉瓣合并二尖瓣钙化患者次之(17.1%),单纯二尖瓣钙化者较少(6.0%)。既往研究也报道了此类患者心脏瓣膜钙化以主动脉瓣钙化多见[7]。
尿毒症患者机体长期处于慢性炎症及缺血缺氧内环境,可通过多种机制发生血管钙化。尿毒症血管钙化以血管的中膜钙化及心脏瓣膜钙化最为常见,并随着肾功能下降临床表现愈发明显,临床可见胸闷气短、乏力、疼痛、钙化防御导致的皮肤软组织损伤破溃、体位性低血压,甚至心源性猝死等。血管钙化在透析患者中发生率最高,也是导致透析患者心血管事件死亡的首要诱因[8-9],是目前透析管理中亟待解决的难题。临床中缺少对尿毒症血管钙化的有效防治手段,近年来一些动物实验研究发现中药治疗可防治血管钙化[10-13],对中医证候的探索却鲜有报道。因此,从中医角度出发进行辨证论治或可成为破解此难治性疾病的关键。
血管钙化可归于中医学的“胸痹”“脉痹”等范畴。现代研究学者通过结合腹膜透析合并血管钙化患者的相关临床表现对其定义及病因病机进行诠释。柳诗意等[14]认为在肾虚本虚标实的基础上,一方面由于肾虚精亏、髓海不足导致骨失所养,另一方面由于浊毒弥漫损伤筋骨、血脉,致使脾肾亏虚,浊毒弥漫,瘀血阻滞,瘀毒互结,痹阻血脉,得出本病的主要证候特征为因虚致瘀,瘀血浊毒交阻。本研究显示腹膜透析合并血管钙化患者的本虚证分布规律以脾肾阳虚证为主,其次为气阴两虚证、脾肾气虚证、肝肾阴虚证和阴阳两虚证;标实证以湿热证为主,其次为湿浊证、血瘀证和水气证,风动证少见。此外,不同年龄组患者的中医证候构成比分布存在差异,50~65岁及66~80岁的患者都存在脾肾阳虚证表现,标实证均以湿热证为主。但66~80岁的患者脾肾阳虚证占比更多,且血瘀证也更突出。透析龄超过26个月的患者本虚证亦表现为脾肾阳虚证为主。该结果符合临床辨证规律,即年龄越大,透析时间愈久,脏腑虚损越严重,而肾衰患者易导致体内水液滞留,体内水液又因停留愈久,化湿生热,从而导致湿热内蕴。亦符合我们对本病的认识,本中心杨洪涛教授[15]认为腹膜透析患者肾脏衰败延及五脏,以阳气亏虚为本,以痰浊、瘀血阻滞为标,而痰浊、瘀血两者不仅是正虚所致的病理产物,又可反过来进一步损伤正气,从而导致血管钙化等心血管并发症的发生。因此治疗本病当以振奋心肾之阳为关键,既要注重补益脾肾二脏,使人体的阳气得到充养,又要注重祛除痰浊、血瘀之实邪,从而使邪去正安,达到治疗疾病的效果。
本研究结果亦提示在临床辨证论治中应当参考相关实验室指标等临床要素,如血红蛋白、血浆白蛋白偏低患者脾肾阳虚证占比大,而血红白蛋和白蛋白是透析患者营养状况评估的重要指标[16-17];提示营养状态差的患者阳虚证愈加明显;血肌酐较高的患者脾肾阳虚愈多,而肌酐偏低的患者以湿热证表现为主。尿毒症腹膜透析患者血管钙化的病机复杂,有肾衰及透析因素的叠加,在临证中当辨病与辨证相结合,抓住患者临床特征与疾病证候规律综合辨证才能精准遣方用药。
本研究通过分析尿毒症腹膜透析伴血管钙化患者的中医证候特征,及其与年龄、性别、透析龄、生化指标等临床要素间的关系,初步探索了本病的证候规律。但尿毒症腹膜透析患者血管钙化的临床表现多样,病机复杂,故对中医证候的研究可进一步拓宽范围,扩增样本量,以便于更好地为临床治疗尿毒症血管钙化提供临床辨证施治依据。
| [1] |
JAGER D, DINANDA J. Cardiovascular and noncardiovascular mortality among patients starting dialysis[J]. JAMA, 2009, 302(16): 1782-1789. DOI:10.1001/jama.2009.1488 |
| [2] |
LONDON G M, GUERIN A P, MARCHAIS S J, et al. Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality[J]. Nephrol Dial Transplant, 2003, 18(9): 1731-1740. DOI:10.1093/ndt/gfg414 |
| [3] |
LIU Z H, YU X Q, YANG J W, et al. Prevalence and risk factors for vascular calcification in Chinese patients receiving dialysis: baseline results from a prospective cohort study[J]. Current Medical Research and Opinion, 2018, 34(8): 1491-1500. DOI:10.1080/03007995.2018.1467886 |
| [4] |
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder(CKD-MBD)[J]. Kidney International Supplements, 2017, 7(1): 1-59. DOI:10.1016/j.kisu.2017.04.001 |
| [5] |
KAUPPILA L I, POLAK J F, CUPPLES L A, et al. New indices to classify location, severity and progression of calcific lesions in the abdominalaorta: a 25-year follow-up study[J]. Atherosclerosis, 1997, 132(2): 245-250. DOI:10.1016/S0021-9150(97)00106-8 |
| [6] |
郑筱萸. 中药新药临床研究指导原则(试行)[M]. 中国医药科技出版社, 2002: 163-168. ZHENG X Y. Guiding principles for clinical research of New TCM drugs(Trial)[M]. Beijing: China Medical Science Press, 2002: 163-168. |
| [7] |
WANG C, JIANG L, FENG S, et al. Risk factor analysis of calcification in aortic and mitral valves in maintenance peritoneal dialysis patients[J]. Kidney & blood pressure research, 2013, 37(4-5): 488-495. |
| [8] |
NELSON A J, RAGGI P, WOLF M, et al. Targeting vascular calcification in chronic kidney disease[J]. JACC Basic to Translational Science, 2020, 5(4): 398-412. DOI:10.1016/j.jacbts.2020.02.002 |
| [9] |
KAKANI E, ELYAMNY M, AYACH T, et al. Pathogenesis and management of vascular calcification in CKD and dialysis patients[J]. Semin Dial, 2019, 32(6): 553-561. DOI:10.1111/sdi.12840 |
| [10] |
柳诗意, 张宁, 孟祥飞, 等. 补肾活血方通过调节OPG/RANK/RANKL系统对慢性肾脏病大鼠血管钙化的抑制作用[J]. 中华中医药杂志, 2016, 31(5): 1652-1658. LIU S Y, ZHANG N, MENG X F, et al. Inhibiting effect of Bushen Huoxue Decoction on vascular calcification in rats with chronic kidney disease by regulating OPG/RANK/RANKL system[J]. China Journal of Traditional Chinese Medicine and Pharmacy, 2016, 31(5): 1652-1658. |
| [11] |
石凯峰, 张宁, 柳诗意, 等. 补肾活血方通过调节Bcl-2/Bax凋亡相关蛋白对慢性肾脏病大鼠血管钙化的影响[J]. 中华中医药杂志, 2017, 32(5): 2188-2193. SHI K F, ZHANG N, LIU S Y, et al. Effects of regulating Bcl-2/Bax apoptosis related protein on vascular calcification by Bushen Huoxue Decoction in chronic kidney disease rats[J]. China Journal of Traditional Chinese Medicine and Pharmacy, 2017, 32(5): 2188-2193. |
| [12] |
HE H Q, LAW B Y K, ZHANG N, et al. Bavachin protects human aortic smooth muscle cells against β-glycerophosphate-mediated vascular calcification and apoptosis via activation of mtor-dependent autophagy and suppression of β-catenin signaling[J]. Front Pharmacol, 2019, 10: 1427. DOI:10.3389/fphar.2019.01427 |
| [13] |
WANG X Q, ZOU X R, ZHANG Y C. From "kidneys govern bones" to chronic kidney disease, diabetes mellitus, and metabolic bone disorder: a crosstalk between traditional Chinese medicine and modern science[J]. Evid Based Complement Alternat Med, 2016, 2016: 4370263. |
| [14] |
柳诗意, 张宁. 慢性肾脏病血管钙化中西医治疗进展[J]. 中国中西医结合杂志, 2017, 37(10): 1276-1280. LIU S Y, ZHANG N. Progress of traditional Chinese and western medicine treatment of vascular calcification in chronic kidney disease[J]. Chinese Journal of Integrated Traditional and Western Medicine, 2017, 37(10): 1276-1280. DOI:10.7661/j.cjim.20170721.191 |
| [15] |
姜晨, 杨洪涛. 杨洪涛教授运用中医药在腹膜透析治疗中的经验[J]. 中国中西医结合肾病杂志, 2014, 15(4): 287-289. JIANG C, YANG H T. Professor Yang Hongtao's experience in peritoneal dialysis treatment with traditional Chinese medicine[J]. Chinese Journal of Integrated Traditional and Western Nephrology, 2014, 15(4): 287-289. |
| [16] |
KIEBALO T, HOLOTKA J, HABURA I, et al. Nutritional status in peritoneal dialysis: nutritional guidelines, adequacy and the management of malnutrition[J]. Nutrients, 2020, 12(6): 1715. DOI:10.3390/nu12061715 |
| [17] |
周胜元, 刘玥, 侯长青, 等. 基于不同虚证分型的ESRD血透患者透析前后的营养状态变化研究[J]. 天津中医药, 2019, 36(9): 860-864. ZHOU S Y, LIU Y, HOU C Q, et al. Study on the changes of nutritional state of ESRD patients before and after hemodialysis based on different types of deficiency syndrome[J]. Tianjin Journal of Traditional Chinese Medicine, 2019, 36(9): 860-864. |
2. Department of Nephrology, Heze Traditional Chinese Medicine Hospital, Heze 274000, China;
3. Department of Emergency, Second Affiliated Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300250, China
 2021, Vol. 38
2021, Vol. 38




