文章信息
- 赵玉珂, 陆峰, 范晓艳
- ZHAO Yuke, LU Feng, FAN Xiaoyan
- 升陷汤加味联合西医综合治疗慢性心力衰竭气虚血瘀证患者的临床疗效观察
- Clinical observation on the combined treatment of qi asthenia causing blood stasis syndrome patients in chronic heart failure with Modified Shengxian Decoction and Western medicine
- 天津中医药, 2022, 39(11): 1367-1372
- Tianjin Journal of Traditional Chinese Medicine, 2022, 39(11): 1367-1372
- http://dx.doi.org/10.11656/j.issn.1672-1519.2022.11.02
-
文章历史
- 收稿日期: 2022-07-20
2. 山东中医药大学附属医院心血管病一科, 济南 250014
慢性心力衰竭(CHF)是各种原因导致的心脏结构或功能异常,心室射血能力或充盈受损进而静脉血液淤阻、组织灌注低下,表现为呼吸困难、运动耐量降低、四肢乏力、液体潴留等。CHF是心脏疾病最严重且终末的阶段,预后较差,不断优化的西医治疗由过去强调减轻症状转变为以防治、延缓心肌重构为主,但CHF的病死率、再住院率及长期预后并未明显改观。中医称CHF为“心衰病”,近年来,中医药联合西医综合治疗“心衰病”积累了丰富的经验,疗效优于单纯西医治疗。宗气是全身气血的纲领,宗气不足进而下陷,津血不行则水饮、瘀血内生,心肺功能特别是心功能障碍,心肌变厚甚至心肌重塑,变生一系列“心衰病”证候。针对其病机,益气升阳、活血利水法可减轻CHF气虚血瘀证患者的临床症状,改善心功能[1]。本研究观察升陷汤加味联合西医综合治疗CHF气虚血瘀证患者治疗前后的症状及心功能,评价升陷汤加味的临床疗效。
1 资料和方法 1.1 一般资料选取2020年6月—2021年5月于山东中医药大学附属医院心血管病一科门诊或住院治疗的60例CHF气虚血瘀证患者,纳入标准:1)西医诊断标准参考《中国心力衰竭诊断和治疗指南2018》[2],纽约心脏病协会(NYHA)分级Ⅱ级或Ⅲ级。2)中医辨证气虚血瘀证参考《中药新药临床研究指导原则(试行)》[3],主症:心前区憋闷疼痛,气短,颈部青筋明显,心悸怔忡,胁下癥积,肢体凹陷性水肿,舌有瘀斑或舌质紫黯,脉结代或脉涩;次症:疲倦,喘促,乏力,面容晦滞,咳嗽有痰,口干,眩晕等。3)一般状况尚可,合并疾病稳定。4)患者知情同意并签署相关文书。排除标准:1)病情不稳定或存在增加死亡风险的因素如:梗阻性心肌病、高度房室传导阻滞、急性心肌梗死、心包填塞、缩窄性心包炎、感染性心内膜炎等。2)合并精神类疾病、肝肾功严重不全、恶性肿瘤、结核的患者。3)妊娠期、哺乳期妇女。4)意识障碍无法沟通的患者。5)接受其他中药或中成药试验,可能影响结果者。按照随机数字表法分为对照组和治疗组,每组30例。对照组男16例,女14例;年龄49~88岁,平均(70.40±9.28)岁;心功能Ⅱ级17例,心功能Ⅲ级13例。治疗组男15例,女15例;年龄42~89岁,平均(67.47±12.46)岁;心功能Ⅱ级19例,心功能Ⅲ级11例。本方案经医院伦理委员会审核通过,批件号:JMLL20200522。两组患者临床基线资料相比,差异均无统计学意义(P>0.05)。
1.2 治疗方法两组患者均予低脂低盐饮食,注意休息,避免劳累,病情需要时可氧疗,关注酸碱平衡、电解质、每日体质量变化及尿量。对照组参考《心力衰竭合理用药指南(第2版)》[4],予血管紧张素受体-脑啡肽酶抑制剂(ARNI)沙库巴曲缬沙坦钠片(国药准字H20170364)50 mg或100 mg每日2次;β受体阻滞剂琥珀酸美托洛尔缓释片(国药准字J20150044)23.75 mg或47.5 mg每日1次;醛固酮受体拮抗剂(ARA)螺内酯片(国药准字H32020077) 20 mg每日1次;根据病情决定是否需加用钠-葡萄糖协同转运蛋白2抑制剂(SGLT2i)、伊伐布雷定、洋地黄类、血管扩张药物,并对CHF危险因素进行控制。治疗组在对照组治疗基础上加服升陷汤加味,组方:生黄芪40 g,知母15 g,升麻6 g,柴胡6 g,当归15 g,桔梗9 g,丹参15 g,三七3 g(冲服),桂枝15 g,党参15 g,炒白术15 g,茯苓15 g。气虚兼阳虚者,党参改红参9 g;阴虚内热者,党参改西洋参15 g;心悸怔忡者加磁石、生龙骨、生牡蛎各30 g(先煎);畏寒肤冷去知母加补骨脂、菟丝子各15 g。每日1剂,水煎至400 mL,早晚温服,治疗4周。
1.3 观察指标1) Lee氏心衰评分:劳力性呼吸困难、夜间阵发性呼吸困难、端坐呼吸或夜间咳嗽、休息时也可出现分别计1、2、3、4分;一侧肺底啰音、两侧肺底啰音、啰音不仅限两肺底分别计1、2、3分;轻、中、重度水肿分别计1、2、3分;肝脏肿大肋下触及小于1.5 cm、1.5~3 cm、大于3 cm分别计1、2、3分;颈静脉充盈、肝颈静脉回流征(+)均计1分、颈静脉零水平3 cm及以上计2分;胸片示肺淤血、肺间质水肿、胸腔积液合并肺水肿各计1、2、3分。2)中医证候评分:参考《中药新药临床研究指导原则(试行)》[3]评定,症状按无、轻、中、重,记0、2、4、6分。3)左室射血分数(LVEF):治疗前后各测量1次LVEF。4)实验室检查:治疗前后各化验1次血清N末端B型利钠肽原(NT-proBNP)。
1.4 疗效标准1) 心功能疗效标准:根据Lee心衰评分法,治疗后评分减少≥75%认为显效;评分减少≥50%且<75%认为有效;评分减少<50%认为无效;评分超过治疗前认为恶化。2)中医证候疗效标准:治疗后中医证候疗效评分减少≥70%认为显效;评分减少≥30%且<70%认为有效;评分减少<30%认为无效;评分超过治疗前认为恶化。
1.5 统计学方法应用SPSS 23.0进行统计学分析,Lee氏心衰评分、中医证候评分、LVEF、血清NT-proBNP等计量资料用(x±s)表示,比较应用t检验;临床有效率属计数资料比较应用χ2检验,P<0.05为差异有统计学意义。
2 结果 2.1 两组心功能疗效比较治疗组心功能疗效有效率93.34%(28/30)高于对照组66.67%(20/30),差异有统计学意义(χ2=6.667,P<0.05)。见表 1。
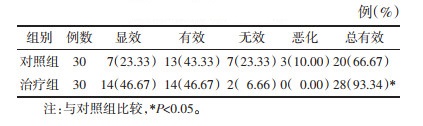
|
治疗组中医证候疗效有效率96.67%(29/30)高于对照组70.00%(21/30),差异有统计学意义(χ2=7.680,P<0.05)。见表 2。
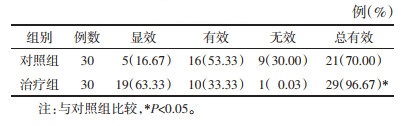
|
两组治疗后Lee氏心衰评分和中医证候疗效评分均较前降低,差异均有统计学意义(P<0.05);治疗组患者治疗后Lee氏心衰评分和中医证候评分均低于对照组,差异均有统计学意义(P<0.05)。见表 3。
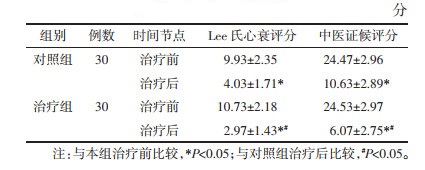
|
两组患者治疗后LVEF较前升高,血清NT-proBNP水平较前降低,差异均有统计学意义(P<0.05);治疗组患者治疗后LVEF高于对照组,血清NT-proBNP水平低于对照组,差异均有统计学意义(P<0.05)。见表 4。
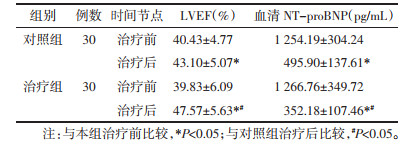
|
研究显示,CHF是世界发病率、病死率增加的首要原因,影响世界约6 400万人[5]。中国35岁以上人群约1.3%患有CHF,人数达890万人[6]。随访4.7年中83%的CHF患者至少住院1次,且出院后1个月内再住院率达20%~30%[7]。从以往ARA、血管紧张素转化酶抑制剂(ACEI)/血管紧张素Ⅱ受体拮抗剂(ARB)、β受体阻滞剂组成的“金三角”到ARNI优化的新“金三角”,再到加用SGLT2i的“新四联”治疗方案的演变,给CHF患者带来更多更好的获益[8],虽然治疗不断优化,但由于利尿剂抵抗、反复严重的电解质紊乱、肾功能进行性恶化、老年衰弱状态、难以去除病因等并没有显著改善患者的长期预后[9]。中医药可在多靶点、多途径干预调治CHF,在整体、宏观、辨证基础上,认识病机结合探索个体、生物、心理等现代领域,是治疗CHF的一种全新的突破[10]。因此加载中医药治疗CHF可更理想地改善患者中医证候及生活质量,减少复发,对远期疗效极具意义[11]。
“心衰病”的形成机制和宗气密切相关,侯瑞等[12]研究《黄帝内经》中“胃之大络”的相关条文,根据心脏结构推演出“虚里”即心脏,是胃之大络,认为心衰病的病位在“虚里”。张锡纯云:“是大气者,原以元气为根本,以水谷之气为养料,以胸中之地为宅窟”,阐释了宗气源于先天之精,得后天水谷精微、清气充养,并描述其功用及地位:“诚以能撑持全身,为诸气之纲领”“为后天生命之宗主”[13]。宗气主要生理功能包括:走息道行呼吸,是“呼吸之枢机”[14];贯心脉行血气,“心以血为主,赖有大气流行以运用之,乃能鼓荡周旋,无微不至”,鼓舞心脏搏动、调节心率和心律[15];亦可“斡旋全身,统摄三焦”,调节水液的生成和敷布。“心衰病”表现为虚实夹杂之证,心气虚、阳虚、水停、血瘀4种基本证型组合、演变,并互为因果、恶性循环,但其核心是宗气失调、甚则下陷[16]。宗气亏陷,升举不能,“呼吸之气不能上达,胸中之气息息下坠”,表现为呼吸困难,胸闷坠胀、心悸等气虚气陷之症。宗气不足、气不行血,又宗气不能贯心脉可直接导致心脏功能减退[17],表现为口唇青紫、颈部青筋暴露、胁下癥积等瘀血征。气机升降失司,不能通调水道,水液泛滥肌肤则水肿尿少,甚则出现胸水、腹水。结合“血不利则为水”的观念,一方面,瘀血阻滞气机,水饮内停;另一方面,血液不循常道溢于脉外,输布失常,成为“病水”,而水停也加重瘀血状态,因此血、水同为病理产物,也为致病因素,更相因为病[18]。
张锡纯首创大气下陷理论,用益气升阳举陷法治疗“心衰病”气虚气陷证,创立的升陷汤疗效显著。本研究针对“心衰病”心气虚、阳虚、水停、血瘀并存的病机,在升陷汤基础上加用活血利水之品,功在益气升阳、活血利水,标本兼治、邪正兼顾。方中黄芪益气升气,为君药;知母甘凉质润,制约黄芪温燥之性防伤阴液和气升太过,为佐制药;柴胡入少阳经,引气陷从左升,升麻入阳明,引气陷从右升,为臣药;桔梗载药上行至胸中,使气息得续,津液得化,为使药。原方基础上加当归、三七养血活血、祛瘀定痛;丹参养血活血、清心凉血安神;桂枝辛温,一取其条达宣通,功可升陷,二则味辛,通于秋气,善降逆,可平肝木,因此缘肝而上之气桂枝可都镇之,三则助阳化气行水;茯苓利水健脾宁心;党参、白术健脾利水。诸药共奏益气举陷升阳、活血通脉利水之功。现代药理研究表明,中药通过增加心肌细胞收缩、抗氧化、减轻心脏前后负荷等治疗CHF,与“强心、利尿”治疗原则相吻合[19]。黄芪中黄芪多糖、黄体酮、生物碱等,增强心肌收缩,使心肌细胞耗氧量降低,正性肌力效果明显,可优化心肌代谢,延缓心肌重构,改善LVEF[20-21];柴胡通过作用于CHF大鼠体内长链脂肪酸、肉碱含量提高心血管功能[22];桔梗根部的提取物能够调节多种促炎介质[23-24],减缓CHF进展,亦可降低毛细血管通透性,缓解水钠潴留;升麻可抗炎镇痛,能显著改善胸痛症状;知母中知母皂苷影响血管内皮细胞功能及血小板聚集;丹参中丹参素、丹参酮等能保护内皮细胞,扩张冠状动脉,降低自由基和炎性因子引起的细胞损害,并调节心肌细胞膜钙、钾离子通道,抑制细胞凋亡,且可抑制心肌重构[25],阻滞血小板聚集,降低血液黏稠度及血栓风险;当归挥发油可增加心排血量,减低氧耗,延长心肌细胞凋亡时间,改善缺血后再灌注损伤;三七中槲皮素具强心功效,黄酮对抗T波改变从而改善缺血状态;党参可减轻心肌细胞的缺血性损害,减缓细胞氧化,通过增加葡萄糖利用优化心肌能量代谢,并在不影响心率的情况下增加心脏排血量,增强运动耐量[26];茯苓素可拮抗醛固酮受体,改善心肌运动及体内水液代谢;桂枝可改善血管内皮舒张发挥扩血管作用。
本研究在西医标准治疗基础上,联合升陷汤加味治疗CHF 4周后,治疗组心功能有效率、中医证候疗效有效率高于对照组,两组Lee氏心衰评分、中医证候疗效评分均较前降低,治疗组降低更明显,提示升陷汤加味应用于CHF可有效改善患者主观症状及体征,提高生活质量和活动能力。LVEF是评估左心室收缩功能的关键指标,水平越低,心肌坏死及心室重构越明显[27]。本研究结果表明,治疗后两组患者LVEF均增加,但治疗组增加更明显,提示升陷汤加味可改善患者心功能、增强心肌收缩力。血清NT-proBNP是国际及国内CHF指南首选推荐的标志物,作为血脑钠肽(BNP)裂解的氨基末端片段,相比BNP更具稳定性、半衰期更长、浓度更高,在心室容量和压力负荷增大时,其浓度快速上升[28],研究表明,血清NT-proBNP水平和心室扩张严重程度呈现正相关,是CHF独立预后评价指标之一[29-30]。本研究结果显示治疗后两组患者血清NT-proBNP水平均降低,但治疗组降低更明显,提示升陷汤加味联合西医综合治疗比单纯西医治疗抗心力衰竭效果更佳。
本研究的不足在于样本量较小、观察时间较短,未进行多中心临床研究,尚需大规模研究进一步证实完善;另外在患者病情程度、基础疾病、饮食、生活方式、情绪等各种因素作用下,研究过程中可能出现证型的变化,未将此因素考虑在内。综上,针对CHF气虚血瘀证患者,升陷汤加味联合西医综合治疗可明显改善患者主观症状和体征,提高生活质量,降低血清NT-proBNP水平,提高LVEF,改善心功能。升陷汤加味运用于心血管疾病开拓了中医药防治CHF的治疗思路,一定程度上提供了中西医结合治疗CHF的循证证据,值得推广和进一步研究。
| [1] |
王国倩, 喻敏成, 喻正科, 等. 中医药干预舒张性心力衰竭的研究进展[J]. 中国中医药信息杂志, 2016, 23(9): 130-133. WANG G Q, YU M C, YU Z K, et al. Research progress in TCM intervention in diastolic heart failure[J]. Chinese Journal of Information on Traditional Chinese Medicine, 2016, 23(9): 130-133. DOI:10.3969/j.issn.1005-5304.2016.09.032 |
| [2] |
中华医学会心血管病学分会心力衰竭学组, 中国医师协会心力衰竭专业委员会, 中华心血管病杂志编辑委员会. 中国心力衰竭诊断和治疗指南2018[J]. 中华心血管病杂志, 2018, 46(10): 760-789. Heart Failure Group of Chinese Society of Cardiology, Heart Failure Professional Committee of Chinese Medical Doctor Association, Editorial Committee of Chinese Journal of Cardiology. Chinese guidelines for diagnosis and treatment of heart failure[J]. Chinese Journal of Cardiology, 2018, 46(10): 760-789. DOI:10.3760/cma.j.issn.0253-3758.2018.10.004 |
| [3] |
郑筱萸. 中药新药临床研究指导原则[M]. 北京: 中国医药科技出版社, 2002: 77-85. ZHENG X Y. Guiding principles for clinical research of new Chinese medicine drugs[M]. Beijing: China Medical Science Press, 2002: 77-85. |
| [4] |
心力衰竭合理用药指南(第2版)[J]. 中国医学前沿杂志(电子版), 2019, 11(7): 1-78. Guidelines for rational drug use in heart failure (2nd edition)[J]. Chinese Journal of the Frontiers of Medical Science (Electronic Version), 2019, 11(7): 1-78. |
| [5] |
BRAGAZZI N L, ZHONG W, SHU J X, et al. Burden of heart failure and underlying causes in 195 countries and territories from 1990 to 2017[J]. European Journal of Preventive Cardiology, 2021, 28(15): 1682-1690. DOI:10.1093/eurjpc/zwaa147 |
| [6] |
HAO G, WANG X, CHEN Z, et al. Prevalence of heart failure and left ventricular dysfunction in China: the China hypertension survey, 2012-2015[J]. European Journal of Heart Failure, 2019, 21(11): 1329-1337. DOI:10.1002/ejhf.1629 |
| [7] |
ORSO F, FABBRI G, MAGGIONI A P. Epidemiology of heart failure[J]. Handbook of Experimental Pharmacology, 2017, 243: 15-33. |
| [8] |
吴章民, 杨成明, 曾春雨. 沙库巴曲缬沙坦联合SGLT2抑制剂对心力衰竭的影响作用[J]. 中国循证心血管医学杂志, 2022, 14(1): 116-117. WU Z M, YANG C M, ZENG C Y. Influence of sakubatril-valsartan combined with SGLT2 inhibitor on heart failure[J]. Chinese Journal of Evidence-Based Cardiovascular Medicine, 2022, 14(1): 116-117. DOI:10.3969/j.issn.1674-4055.2022.01.30 |
| [9] |
赵玲, 马丹, 刘凤歧. 脑啡肽酶及其抑制剂在心力衰竭治疗中的研究概述[J]. 中华老年多器官疾病杂志, 2022, 21(1): 63-66. ZHAO L, MA D, LIU F Q. Research progress of neprilysin and its inhibitor in treatment of heart failure[J]. Chinese Journal of Multiple Organ Diseases in the Elderly, 2022, 21(1): 63-66. |
| [10] |
朱杰, 林兆奋, 胡聃, 等. 中西医结合治疗慢性心力衰竭研究进展[J]. 陕西中医, 2020, 41(9): 1342-1344. ZHU J, LIN Z F, HU D, et al. Research progress of integrated traditional Chinese and Western medicine in the treatment of chronic heart failure[J]. Shaanxi Journal of Traditional Chinese Medicine, 2020, 41(9): 1342-1344. DOI:10.3969/j.issn.1000-7369.2020.09.046 |
| [11] |
尼苦王康, 邓兵. 中药治疗射血分数保留的心力衰竭研究进展[J]. 陕西中医, 2022, 43(3): 405-408. NI K W K, DENG B. Research progress of traditional Chinese medicine in treating heart failure with preserved ejection fraction[J]. Shaanxi Journal of Traditional Chinese Medicine, 2022, 43(3): 405-408. DOI:10.3969/j.issn.1000-7369.2022.03.033 |
| [12] |
侯瑞, 王燕, 张久亮. 从《黄帝内经》对"虚里"的论述探讨心力衰竭的治疗要点[J]. 中华中医药杂志, 2020, 35(9): 4328-4330. HOU R, WANG Y, ZHANG J L. Investigation on the key point of treating heart failure from the discussion of xuli in Huangdi Neijing[J]. China Journal of Traditional Chinese Medicine and Pharmacy, 2020, 35(9): 4328-4330. |
| [13] |
张锡纯. 医学衷中参西录[M]. 石家庄: 河北人民出版社, 1974: 32-34. ZHANG X C. Yixue Zhongzhong Canxilu[M]. Shijiazhuang: Hebei People's Publishing House, 1974: 32-34. |
| [14] |
温武兵, 张珍玉. 论宗气的生理功能[J]. 山东中医药大学学报, 2000, 24(4): 247-250. WEN W B, ZHANG Z Y. On the physiological function of thoracic qi[J]. Journal of Shandong University of Traditional Chinese Medicine, 2000, 24(4): 247-250. DOI:10.3969/j.issn.1007-659X.2000.04.002 |
| [15] |
李永民, 杨洁, 王陶冶. 中药心衰康治疗慢性充血性心力衰竭经验简介[J]. 陕西中医, 2004, 25(7): 658. LI Y M, YANG J, WANG T Y. Chinese medicine Xinshuaikang treatment of chronic congestive heart failure experience brief introduction[J]. Shaanxi Journal of Traditional Chinese Medicine, 2004, 25(7): 658. DOI:10.3969/j.issn.1000-7369.2004.07.063 |
| [16] |
李忠业. 论温养宗气法治疗心衰病的意义[J]. 中医药通报, 2012, 11(6): 41-43. LI Z Y. Discussion on the significance of warming and nourishing qi in the treatment of heart failure[J]. Traditional Chinese Medicine Journal, 2012, 11(6): 41-43. |
| [17] |
胡增. 升补宗气法治疗慢性心力衰竭的临床应用[D]. 沈阳: 辽宁中医药大学, 2014. HU Z. Clinical application of raising and replenishing thoracic qi method in the treatment of chronic heart failure[D]. Shenyang: Liaoning University of Traditional Chinese Medicine, 2014. |
| [18] |
隋艳波, 凌丽云, 刘莉. "血不利则为水"理论论治心力衰竭研究[J]. 陕西中医, 2021, 42(2): 213-216. SUI Y B, LING L Y, LIU L. Treating heart failure based on the theory of "unsmooth blood circulation results in water"[J]. Shaanxi Journal of Traditional Chinese Medicine, 2021, 42(2): 213-216. DOI:10.3969/j.issn.1000-7369.2021.02.019 |
| [19] |
王转转. 长期口服芪红汤对慢性心力衰竭患者左心室重构、MMP-9及NP-proBNP的影响[J]. 陕西中医, 2017, 38(2): 165-166. WANG Z Z. Effect of long-term oral Qihong Decoction on left ventricular remodeling, MMP-9 and NP-proBNP in patients with chronic heart failure[J]. Shaanxi Journal of Traditional Chinese Medicine, 2017, 38(2): 165-166. |
| [20] |
李幼萍, 肖忠英, 倪卫. 黄芪保心汤联合比索洛尔治疗射血分数保留型心力衰竭疗效及对患者心功能的影响[J]. 陕西中医, 2020, 41(10): 1399-1402. LI Y P, XIAO Z Y, NI W. Clinical efficacy of Huangqi Baoxin Decoction combined with bisoprolol in the treatment of heart failure with preserved ejection fraction and its effects on cardiac function and 6MWT[J]. Shaanxi Journal of Traditional Chinese Medicine, 2020, 41(10): 1399-1402. DOI:10.3969/j.issn.1000-7369.2020.10.016 |
| [21] |
李焱, 姜泽丰, 乔冬卉, 等. 附子-黄芪-葶苈子角药对心力衰竭模型大鼠心肌细胞线粒体膜电位及钙调节蛋白NCX1、SERCA2的影响[J]. 中医杂志, 2021, 62(3): 252-258. LI Y, JIANG Z F, QIAO D H, et al. The Effect of Fuzi, Huangqi, Tingliziherb combination on myocardial mitochondrial membrane potential and calmodulin NCX1 and SERCA2 in heart failure model rats[J]. Journal of Traditional Chinese Medicine, 2021, 62(3): 252258. |
| [22] |
ZHANG F, ZHAN Q, DONG X, et al. Shengxian Decoction in chronic heart failure treatment and synergistic property of Platycodonis Radix: a metabolomic approach and its application[J]. Molecular BioSystems, 2014, 10(8): 2055-63. |
| [23] |
KIM J Y, KIM D H, KIM H G, et al. Inhibition of tumor necrosis factor-alpha-induced expression of adhesion molecules in human endothelial cells by the saponins derived from roots of Platycodon grandiflorum[J]. Toxicology and Applied Pharmacology, 2006, 210(1/2): 150-156. |
| [24] |
LIM D Y, KIM B C, LEE E B. Comparison of vasodilator LVEF fects of platycodin D and D3 in rats[J]. Korean journal of physiology & pharmacology, 2003, 7(3): 149-155. |
| [25] |
赵全如, 谢晓燕. 丹参的化学成分及药理作用研究进展[J]. 广东化工, 2021, 48(1): 57-59. ZHAO Q R, XIE X Y. Research progress of phytochemistry, pharmacological action of Salvia miltiorrhiza[J]. Guangdong Chemical Industry, 2021, 48(1): 57-59. |
| [26] |
张蕊, 陈乃宏. 补益药党参的药理作用研究进展及其在临床上的应用[A]. 中国药理学会补益药药理专业委员会成立大会暨人参及补益药学术研讨会会议论文集[C], 2011: 42. ZHANG R, CHEN N H. Research progress of pharmacological action of tonic medicine Codonopsis pilosula and its clinical application[A]. Proceedings of the Inaugural Meeting of The Professional Committee of Tonic Medicine Pharmacology of Chinese Pharmacological Society and the Symposium on Ginseng and Tonic Medicine[C], 2011: 42. |
| [27] |
YAMAMOTO M, SEO Y, ISHIZU T, et al. Different impact of changes in left ventricular ejection fraction between heart failure classifications in patients with acute decompensated heart failure[J]. Circulation Journal, 2019, 83(3): 584-594. |
| [28] |
周丽华, 杨威, 吉中蛟. 老年慢性心力衰竭患者血清MR-ProADM、miRNA-21水平变化与预后的关系研究[J]. 中国免疫学杂志, 2019, 35(23): 2904-2907, 2910. ZHOU L H, YANG W, JI Z J. Relationship between serum MR-ProADM, miRNA-21 levels and prognosis in elderly patients with chronic heart failure[J]. Chinese Journal of Immunology, 2019, 35(23): 2904-2907, 2910. |
| [29] |
BENES J, KOTRC M, CONRAD M J, et al. Exercise dynamics of cardiac biomarkers and hemoconcentration in patients with chronic systolic heart failure[J]. Journal of Cardiac Failure, 2020, 26(12): 1100-1105. |
| [30] |
SALAH K, STIENEN S, PINTO Y M, et al. Prognosis and NT-proBNP in heart failure patients with preserved versus reduced ejection fraction[J]. Heart (British Cardiac Society), 2019, 105(15): 1182-1189. |
| [31] |
吕玲, 李霖, 李明玥, 等. 中医药治疗慢性心力衰竭评价指标应用现状分析[J]. 天津中医药, 2022, 39(1): 123-130. LYU L, LI L, LI M Y, et al. Analysis of the current situation of application of evaluation indexes of traditional Chinese medicine in the treatment of chronic heart failure[J]. Tianjin Journal of Traditional Chinese Medicine, 2022, 39(1): 123-130. |
2. First Department of Cardiovascular Disease, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250014, China
 2022, Vol. 39
2022, Vol. 39




