文章信息
- 赵启亮, 张东, 范爽, 等.
- ZHAO Qiliang, ZHANG Dong, FAN Shuang, et al.
- 新型冠状病毒感染本土病例中七情过极对脏腑气机影响的研究
- A study on the influence of disordered seven emotions on the qi movement of Zang-fu organs in local COVID-19 patients
- 天津中医药, 2023, 40(8): 955-960
- Tianjin Journal of Traditional Chinese Medicine, 2023, 40(8): 955-960
- http://dx.doi.org/10.11656/j.issn.1672-1519.2023.08.02
-
文章历史
- 收稿日期: 2023-04-24
2. 国家中医针灸临床医学研究中心, 天津 300381;
3. 天津市海河医院结核病科, 天津 300350;
4. 天津中医药大学研究生院, 天津 301617
新型冠状病毒感染(COVID-19)不仅威胁人民群众的生理健康,其对患者心理健康的影响越来越受到重视,诸多研究报道显示,部分新冠患者存在睡眠、抑郁、焦虑等心理问题,制定针对性的心理指导方案,协助患者度过心理危机,能促进患者疾病康复[1-3]。
COVID-19属于“疫病”范畴,中医学历来重视情志致病,“心身合一”的整体观思想影响着中医基本理论的形成,历代医家均把这种心身整体观应用于防治疾病和养生保健的过程中。情志变化存在于COVID-19整个病程中,七情主要影响脏腑气机的升降出入,不同患者临床不同阶段中医七情的特征、脏腑气机的升降出入变化也应存在差异,探析总结七情过极影响脏腑气机变化的规律,有助于指导临床对患者的中医情志诊疗。
1 资料与方法 1.1 病例来源2019年2月—2020年8月,天津市海河医院收治的COVID-19住院确诊患者。研究已通过天津市海河医院医学伦理委员会审批(伦理批件号2020HHKT-026)。
1.2 诊断标准参考国家卫生健康委员会《新型冠状病毒感染的肺炎诊疗方案(试行第七版)》[4]标准拟定。即疑似病例+病原学或血清学证据。
1.3 中医七情的定义参考《中医基础理论》2012版[5],中国中医药出版社。
1)怒:由于愿望受阻、行为受挫而致的紧张情绪的体验。2)喜:伴随愿望实现、紧张情绪解除时的轻松愉快的情绪体验。3)思:对所思问题不解,事情未决,思虑担忧的复合情绪状态。4)悲:人失去所爱之物,及所追求的愿望破灭时的情绪体验。5)恐:遇到危险而又无力应付而引发的惧怕不安的情绪体验。6)惊:突然遭受意料之外的事件而引发的紧张惊骇的情绪体验。7)忧:面临问题的解决看不到头绪,心情低沉并伴有自卑的复合情绪状态。
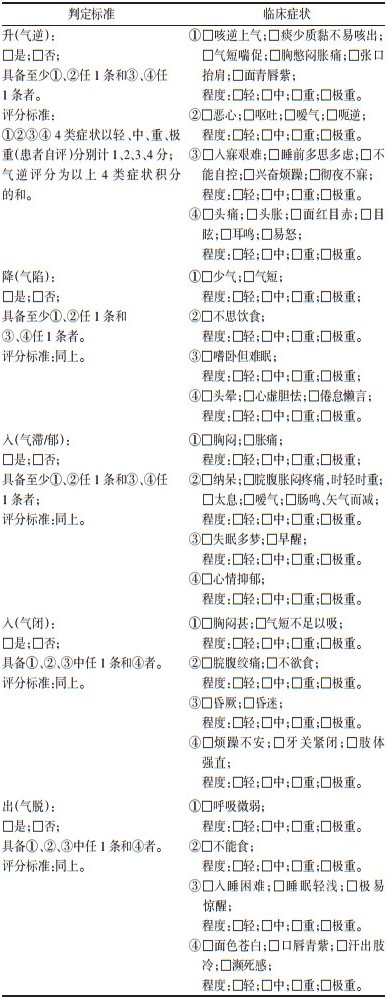
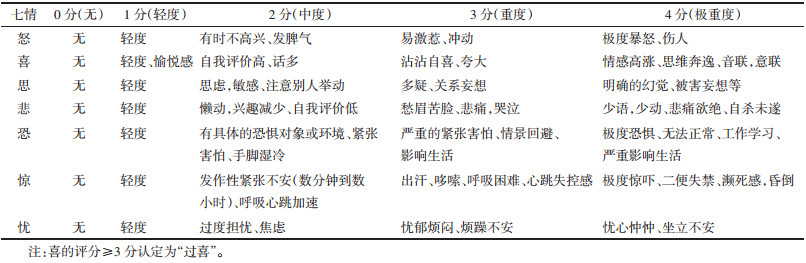
1.4 中医七情过极的评分标准参考《现代中医心理学》2007年版[6],中国中医药出版社。见表 1。
|
参照《中华人民共和国国家标准·中医临床诊疗术语》[7]及《中药新药临床研究指导原则》[8]制定。见表 2。
纳入符合COVID-19疾病诊断标准者;排除既往合并有抑郁症、焦虑症、强迫症等精神疾病者,以及因疾病或其他原因无法配合信息采集者。
1.7 方法采用统一的调查问卷,由具备中医学背景的专职医生采集入院时、住院1周、出院时共3个时点不同临床阶段信息,判定七情及气机升降出入评分。通过频数分析总结不同临床阶段的七情和气机的升降出入的特征,通过问卷评分的重复测量方差分析,评价不同时点七情过极和气机失调的严重程度,采用关联规则分析,探析总结七情影响气机的规律。
1.8 统计学方法采用SPSS 26.0软件和SPSS Modeler18.0软件进行分析。计量资料以均数±标准差(x±s)描述,计数资料采用频数和百分比进行描述,3个时点问卷评分采用重复测量方差分析(Greenhouse-Geisser),七情影响气机的规律采用关联规则分析(Apriori算法)。检验水准为α<0.05。
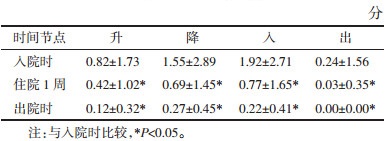
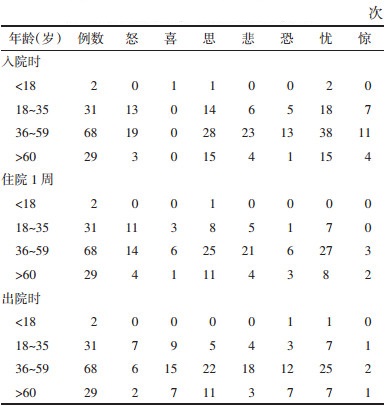
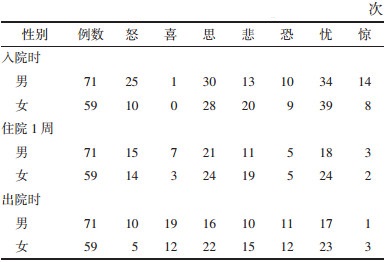
2 结果 2.1 一般情况研究共纳入130例患者,其中男71例(54.62%),女59例(45.38%)。病情分级轻型12例(9.23%),普通型118例(90.77%)。人群年龄范围为9~89岁,平均年龄46.69岁,未成年人(<18岁)2例,老年人(>60岁)29例。不同年龄层患者情志过极主要表现为,未成年人在入院时表现为思和忧,住院1周时仅表现为思,出院时又出现恐;青年人均表现为怒、思、忧;中年人以忧、思、悲、怒、恐为主要表现;老年人以忧、思为主,情志过极均呈逐渐缓解的趋势,见表 3。男性入院时突出表现为怒,其他与女性一样以忧、思为主,见表 4。
|
|
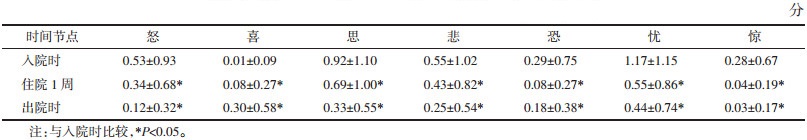
喜不存在过极,其余6种情志过极评分在住院期间均下降,3个时点的差异均有统计学意义(P < 0.05),见表 5。
升、降、入评分在住院期间均呈下降趋势,3个时点的差异均有统计学意义(P < 0.05),见表 6。
入院时,七情特征以忧最常见,脏腑气机特征以入为主;住院1周时七情特征以思最常见,脏腑气机特征以降为主;出院时七情特征以忧为主,脏腑气机特征以降为主,见表 7。
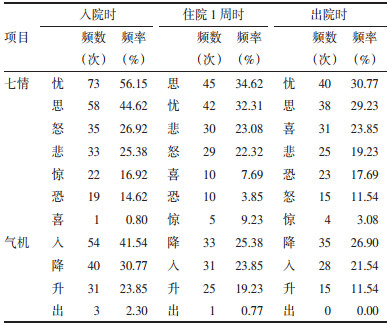
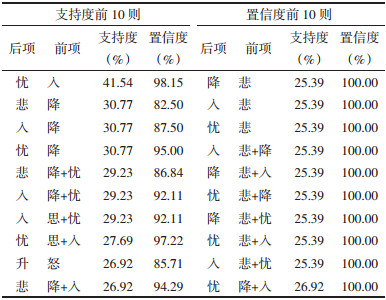
入院时,支持度最高的是入+忧(41.54%),置信度最高的是悲+降/入/忧(100%),见表 8。
|
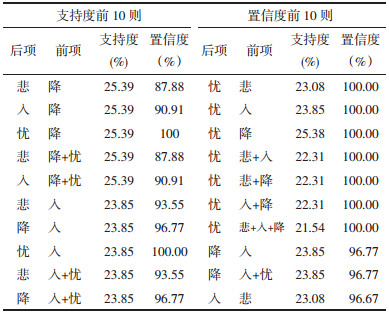
住院1周时,支持度最高的是降+悲/入/忧(25.39%),置信度最高的是悲/入/降+忧(100%),见表 9。
|
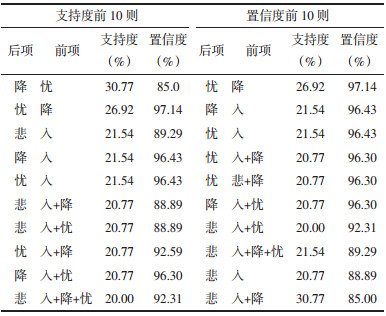
出院时,“忧+降”的支持度(30.77%)和置信度(97.14%)均是最高的,见表 10。
|
COVI-19疫情给人民群众带来了巨大心理压力和精神困扰,及时有效的心理干预,能够促进患者身心早日康复[9]。中医“心身合一”的整体观体现了情志变化对于机体生理及病理变化有影响,中医情志疗法是基于辨证论治的调适、预防和治疗疾病的综合策略。因此,总结COVID-19患者七情和脏腑气机的相互影响及变化规律,可以为临床中医情志致病防治策略优化改进提供参考。
七情包括喜、怒、忧、思、悲、恐、惊,只有当情志刺激超过了人体所能调节的范围,即情志过极,导致气机紊乱、脏腑气血失调而引起疾病发生时,七情才成为致病因素,称为“内伤七情”。七情致病通过影响脏腑气机的运行,最终导致气机运行失常,气血痰瘀郁滞,甚或阴阳失衡,精血亏虚。升、降、出、入是气机运动的基本形式,升、降、出、入运动失常称为“气机失调”。现今中医临床对应以上4种气机失调情况多归结于1)气逆:升太过、降不及。2)气陷:降太过、升不及。3)气郁、气滞、气闭:入太过,出不及。4)气脱:出太过,入不及。综上可知,七情致病病机以脏腑气机的病生理为基础,与其升、降、出、入运动异常密切相关。
3.1 不同阶段七情和气机的特征从患者入院至出院的3个时点中,七情的特征变化趋势为“忧、思、怒、悲”至“思、忧、悲、怒”再至“忧、思、喜、悲”。气机的特征变化趋势为“入、降、升”至“降、入、升”再至“降、入、升”。“忧、思、怒、悲”和“入、降、升”是COVID-19患者住院期间的主要情志-气机表现特征。“忧”主要表现为过度担忧、焦虑、烦闷、坐立不安;“思”表现为思虑过度,敏感多疑;“怒”表现为偶发脾气,易激惹;“悲”表现为懒动,兴趣低,愁眉苦脸。“入”在临床上主要表现为“胸闷、纳呆、失眠多梦、早醒、抑郁”等“气滞”和“气郁”的特征;“降”主要表现为“气短、少气、不思饮食、嗜卧难眠、倦怠懒言”等“气陷”的特征;“升”主要表现为“咳逆上气、痰少质黏难咯、胸闷胀痛、恶心、呕吐、嗳气、入寐艰难、头胀易怒”等“气逆”的特征。与团队前期证候学研究,COVID-19患者初期以呼吸道症状为主,入院后以消化道症状多见,恢复期可见气阴两虚证,病位主要在肺、脾、胃的研究结果相一致[10]。
3.2 七情影响气机升降出入的规律入院时关联规则中,支持度最高的是入+忧(41.54%),置信度最高的是悲+降/入/忧(100%)。住院1周时,支持度最高的是降+悲/入/忧(25.39%),置信度最高的是悲/入/降+忧(100%)。出院时,“忧+降”的支持度(30.77%)和置信度(97.14%)均是最高的。可见,在COVID-19患者住院过程中,七情中“忧”和“悲”导致气机过于“降”和“入”。“忧”和“悲”为肺志,会出现肺气郁闭、耗伤而致气机失调,表现为“气陷于下”,即“气机降太过而升不及”和“气郁于内”,即气机入内太过而外出不及。该研究病例中,大部分患者都是以呼吸道症状为主,病位还是以“肺”最多见,“脾、胃”次之,与研究发现的七情影响气机的规律相符。
综上,天津地区COVID-19患者住院过程中的情志变化主要以“忧、思”为主,气机主要以“入、降”为主,七情中“忧、思”过极导致气机的“入、降”失调,病机表现为肺气升降失司;脾气不升、脾胃失和;气滞于肺、脾、胃。目前尚无从七情角度探讨其对COVID-19患者脏腑气机变化的研究,大多是由于中医七情和气机升降出入的定义和量化判定方式尚无统一的标准,甚至还存在争议,而该研究虽已尽量博采众长,基于患者临床信息,结合中医专家组综合判定的方式求同存异,将观察到的七情与气机的变化规律总结分析如上,该研究结论基于天津地区COVID-19本土确诊患者情况分析,以期为相关研究和临床实践提供参考。
| [1] |
付小宇, 张新雪, 赵宗江. 基于中医情志疗法探讨新冠肺炎疫期的心理调适方法[J]. 中国实验方剂学杂志, 2020, 26(13): 39-44. FU X Y, ZHANG X X, ZHAO Z J. Psychological adjustment during outbreak of COVID-19 based on traditional Chinese medicine emotion therapy[J]. Chinese Journal of Experimental Traditional Medical Formulae, 2020, 26(13): 39-44. |
| [2] |
刘晓彤, 齐向华. 从中医心理紊乱状态探析新冠肺炎的辨治[J]. 国医论坛, 2020, 35(5): 20-22. LIU X T, QI X H. Analysis of COVID-19's differentiation and treatment from the psychological disorder of traditional Chinese medicine[J]. Forum on Traditional Chinese Medicine, 2020, 35(5): 20-22. |
| [3] |
牛鑫, 姚娓. 新型冠状病毒肺炎恢复期抑郁-焦虑-压力及中医五志的调查研究[J]. 实用中医内科杂志, 2021, 35(11): 25-28. NIU X, YAO W. Research on depression-anxiety-stress and five emotions in traditional Chinese medicine of COVID-19 patients in recovery period[J]. Journal of Practical Traditional Chinese Internal Medicine, 2021, 35(11): 25-28. |
| [4] |
国家卫生健康委办公厅, 国家中医药管理局办公室. 关于印发新型冠状病毒感染的肺炎诊疗方案(试行第七版)的通知[EB/OL]. http://www.gov.cn/zhengce/zhengceku/2020-03/04/content_5486705.htm. National Health Commission of the People's Republic of China, National Adminstration of Traditional Chinese Medicine. Notice on the issuance of diagnosis and treatment protocol for novel coronavirus pneumonia (7th edition)[EB/OL]. http://www.gov.cn/zhengce/zhengceku/2020-03/04/content_5486705.htm. |
| [5] |
孙广仁, 郑洪新. 中医基础理论[M]. 3版. 北京: 中国中医药出版社, 2012: 214-215. SUN G R, ZHENG H X. Basic theories of traditional Chinese medicine[M]. 3rd edition. Beijing: China Press of Traditional Chinese Medicine, 2012: 214-215. |
| [6] |
王米渠. 现代中医心理学[M]. 北京: 中国中医药出版社, 2007: 120. WANG M Q. Modern Chinese medicine psychology[M]. Beijing: China Press of Traditional Chinese Medicine, 2007: 120. |
| [7] |
国家技术监督局. 中华人民共和国国家标准中医临床诊疗术语治法部分[S]. 北京: 中国标准出版社, 1997: 3, 24-26, 63-64. The State Bureau of Quality and Technical Supervision. The People's Republic of China national standard traditional Chinese medicine clinical diagnosis and treatment terms[S]. Beijing: Standards Press of China, 1997: 3, 24-26, 63-64. |
| [8] |
郑筱萸. 中药新药临床研究指导原则[S]. 北京: 中国医药科技出版社, 2002: 187. ZHENG X Y. Guidelines for clinical research of new Chinese medicines[S]. Beijing: China Medical Science Press, 2002: 187. |
| [9] |
吕若琳, 周娅楠, 刘立, 等. 从七情学说探讨新冠肺炎防控期间普通民众的心理调护[J]. 心理月刊, 2020, 15(17): 92, 164. LYU R L, ZHOU Y N, LIU L, et al. On the psychological nursing of ordinary people during the prevention and control period in COVID-19 from the theory of seven emotions[J]. Psychological Month, 2020, 15(17): 92, 164. |
| [10] |
孙宏源, 毕颖斐, 朱振刚, 等. 天津地区88例新型冠状病毒肺炎患者中医证候特征初探[J]. 中医杂志, 2020, 61(10): 837-841. SUN H Y, BI Y F, ZHU Z G, et al. Characteristics of traditional Chinese medicine syndromes in 88 patients with coronavirus diseases 2019 in Tianjin[J]. Journal of Traditional Chinese Medicine, 2020, 61(10): 837-841. |
2. National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion, Tianjin 300381, China;
3. Tuberculosis Department, Tianjin Haihe Hospital, Tianjin 300350, China;
4. Graduate School, Tianjin University of Traditional Chinese Medicine, Tianjin 301617, China
 2023, Vol. 40
2023, Vol. 40